After witnessing a close family friend’s seven-year battle with infertility and a failed IVF attempt, I felt compelled to shed light on this important issue. Recently, she made the brave decision to undergo a second IVF treatment, and our entire support system rallied behind her throughout the process. We were actively involved, from the prescription of fertility medications to stimulate egg production to transvaginal ultrasounds to examine the ovaries and regular blood tests to monitor hormone levels. Fortunately, the process proved to be a success, and we were ecstatic with joy.
However, a few weeks later, she experienced some spotting, causing understandable panic. She immediately visited the hospital for a scan, and thankfully, the baby was still safe. Unfortunately, a nightmarish moment ensued when she called, reporting profuse bleeding. She was subsequently admitted to the hospital, where it was revealed that she had lost the baby due to a weak uterine lining. It became evident that weak uterine lining can be a significant factor contributing to female infertility. Women with this condition face tremendous challenges in achieving pregnancy since a thick and healthy uterine lining, also known as the endometrium, is essential for a successful pregnancy and menstrual cycle.
It is crucial to comprehend that if you undergo an IVF procedure with a weak uterine lining, your chances of success may be compromised. The fertilized egg requires a specific thickness of the uterine lining to implant and thrive. However, there is good news. Thin endometrium can be treated through certain lifestyle modifications.
In conclusion, the journey of infertility can be daunting, but understanding the role of uterine lining in IVF success is vital. By addressing and improving the health of the uterine lining, women can enhance their chances of achieving a healthy pregnancy. With ongoing advancements in medical science and lifestyle adjustments, there is hope for those struggling with infertility to realize their dreams of starting a family.
Natural Therapies and Hormonal Balance
Ensuring a healthy and thick uterine lining is crucial for successful IVF outcomes. In this post, we will explore natural therapies that can help increase the thickness and overall health of the endometrium. To understand the workings of the endometrium, it’s important to note that it is the layer shed during menstruation, and estrogen plays a significant role in its thickness.
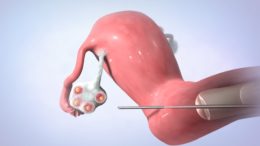
For women undergoing IVF, the thickness of the uterine lining is a vital consideration. Before embryo transfer, doctors must ensure that the lining is adequately thick to support implantation. A thin uterine lining can pose a serious challenge in IVF, potentially leading to failed implantation or pregnancy loss, as in the case of my friend.
Possible Causes of Thin Uterine Lining:
- Low Estrogen:
- The thickness of the endometrium relies on sufficient levels of estrogen. Estrogen is a crucial hormone for sexual and reproductive development, particularly in women. The entire menstrual cycle is dependent on appropriate estrogen levels. In cases of amenorrhea (absent periods), a thin uterine lining due to low estrogen levels is often the cause. Menopause and perimenopause can contribute to low estrogen, resulting in symptoms such as painful sex, irregular or absent periods, urinary tract infections, mood swings, hot flashes, fatigue, and breast tenderness. As women age, hormone levels naturally decline. To evaluate the potential role of a thin uterine lining in infertility, I recommend getting estradiol levels tested and measuring uterine thickness. It’s important to note that estrogen and progesterone work hand in hand.
- Progesterone Imbalance:
- After ovulation, the ovaries secrete progesterone, which helps prepare the body for pregnancy by maintaining the uterine lining for approximately 14 days post-ovulation, facilitating embryo implantation. Progesterone balances and supports the effects of estrogen. When estrogen levels are excessively high and progesterone levels are low, a condition known as estrogen dominance occurs. This hormonal imbalance can lead to negative symptoms, including disruptions in menstrual cycles, reduced chances of conceiving, decreased sex drive, increased PMS symptoms, irregular periods, depression, mood swings, headaches, bloating, hot flashes, breast tenderness, weight gain, fatigue, and difficulty concentrating. In summary, estrogen thins the uterine lining while progesterone maintains it.
Inadequate Blood Flow
Sufficient blood flow plays a vital role in maintaining a thick endometrial lining. The level of blood supply directly impacts the growth and health of the endometrium. Unfortunately, blood flow to the uterus can be compromised for various reasons.
One contributing factor to compromised blood flow is a sedentary lifestyle. As my aunt used to say, there is some truth behind the belief that female bankers have a lower chance of getting pregnant. This can be attributed to the nature of desk jobs and prolonged periods of sitting, which can hinder optimal blood flow to the uterus. To counteract this, I recommend incorporating movement into your daily routine. Taking short brisk walks, engaging in activities like bike rides, and practicing yoga can all help improve blood circulation.
By actively addressing and enhancing blood flow to the pelvic region, you can promote a healthier uterine lining. Remember, small lifestyle changes can make a significant difference in improving your chances of achieving a successful pregnancy.

Uterine Fibroid
Uterine fibroids can disrupt blood flow to the endometrium by pressing on the circulatory area that supplies blood to it. The riskiness of fibroids varies depending on their size and position. Another cause is fibroid embolization, where the blood supply to the fibroid is intentionally cut off to reduce its size. However, this can also reduce blood circulation to certain areas of the uterus, affecting overall blood flow to the uterus.
Stress and its Effects on the Endometrium:
Excessive stress can trigger the sympathetic nervous system, leading to arterial constriction and reduced blood flow to the uterus. This constriction can be detrimental to the endometrium since it heavily relies on the uterine artery for adequate blood supply. Furthermore, stress can disrupt hormonal balance, further affecting the health of the endometrium.
Infection, STDs, and Pelvic Inflammatory Disease:
Bacterial infections, sexually transmitted diseases (STDs), and pelvic inflammatory disease are additional factors that can compromise the health of the endometrial tissue. These conditions can cause inflammation and the formation of scar tissue in the endometrium, leading to dysfunctional endometrial functioning.
Dilation and Curettage (D&C) and its Impact on the Endometrium:
Dilation and curettage is a medical procedure performed to remove tissue from the uterus. While it is used for diagnostic and treatment purposes, incorrect or excessive D&C can result in the removal of the basalis layer of the endometrium. This layer is crucial for endometrial growth, and its absence can cause a condition known as Asherman Syndrome, characterized by the formation of scar tissue in the uterine cavity.
Clomid Usage and its Effect on the Endometrium:
Clomid, also known as clomiphene citrate, is a fertility drug commonly prescribed as the first option for fertility treatment. However, excessive use of Clomid can lead to endometrial thinning. Clomid’s anti-estrogenic properties prevent adequate thickening of the endometrial lining, hindering embryo implantation. Taking breaks of at least six weeks between Clomid cycles is recommended to eliminate the presence of the second isomer, which contributes to endometrial thinning.
Long-term Use of Progestin-based Birth Control:
Progestin, a synthetic form of progesterone, is a hormone used in certain birth control methods. Prolonged use of progestin-based contraceptives has been associated with thinning of the uterine lining. This thinning can affect the endometrium’s ability to support implantation and may impact fertility.
Various factors can influence the health and function of the endometrium. Stress, infections, D&C procedures, excessive Clomid usage, and long-term use of progestin-based birth control methods can all contribute to endometrial thinning or dysfunction. Understanding these effects can aid in developing appropriate interventions and treatments to address underlying causes and improve reproductive outcomes.
Herbs and Supplements to Nourish and Build Thin Uterine Lining
When it comes to addressing the issue of a thin uterine lining, it’s important to consider the role of estrogen levels. Low estrogen can be a contributing factor to this condition. In such cases, one of the wise steps to take is to incorporate foods that can support estrogen levels, known as phytoestrogens, into your diet. Phytoestrogens are natural compounds found in certain plants that mimic the effects of estrogen in the body.
A variety of foods contain phytoestrogens and can help in nourishing and building the uterine lining. Consider including beans, soy products, peas, lentils, pinto beans, whole grains, lima beans, and seeds, especially flaxseed, in your meals. These foods can provide a natural boost to estrogen levels and contribute to the overall health of your uterine lining.
Although it’s important to note that no food actually contains progesterone, there are dietary strategies you can adopt to support your body in producing an optimal amount of progesterone. By consuming a diet rich in specific minerals and nutrients, you can encourage your body’s progesterone production.
To promote progesterone production, focus on incorporating foods that are rich in magnesium, Vitamin B6, and zinc into your meals. These nutrients play crucial roles in hormone regulation and can help your body maintain healthy progesterone levels. Magnesium-rich foods such as leafy green vegetables, nuts, and whole grains, along with sources of Vitamin B6 like bananas, poultry, and fish, can contribute to progesterone synthesis. Additionally, including zinc-rich foods like oysters, lean meats, pumpkin seeds, and legumes in your diet can further support the production of this essential hormone.